A patient care model for scoliosis: causes, how it progresses and lifetime treatment options
By Dr. Derek Lee, DC
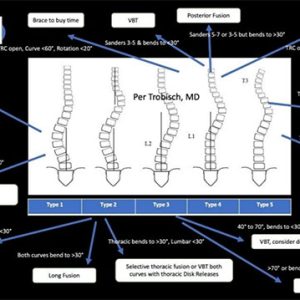
Features Profession Patient Care Techniques adjacent segment degeneration bracing fusion scoliosis spine surgery surgical Vertebral Body Tethering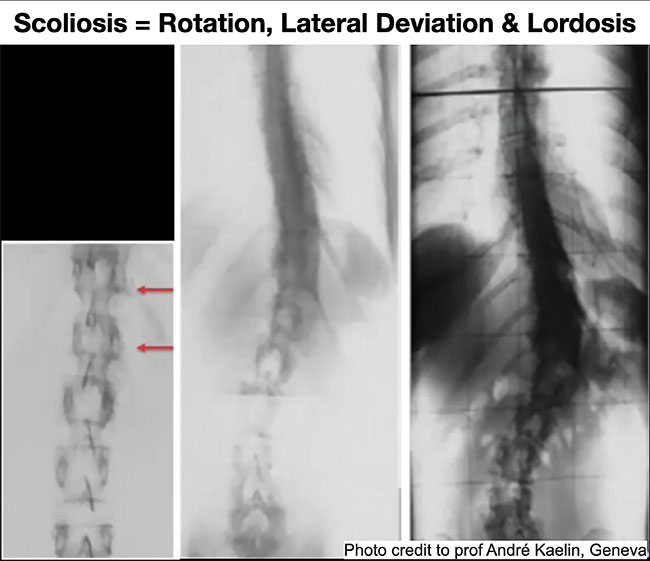 Figure 1 illustrates radiographically how two vertebrae rotate, laterally deviate and progresses to scoliosis.(Professor André Kaelin)
Figure 1 illustrates radiographically how two vertebrae rotate, laterally deviate and progresses to scoliosis.(Professor André Kaelin)
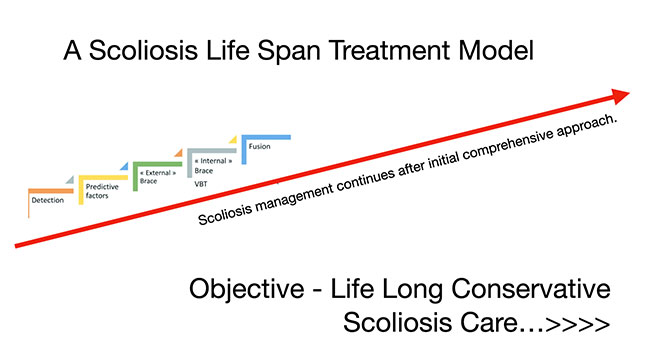
Adolescent Idiopathic Scoliosis (AIS) is a lifelong journey. The difference between early and late detection, diagnosis and treatment of AIS can have significant and chronic health repercussions decades down the road. Right now, scoliosis treatment is mostly narrow in breadth, disconnected among disciplines and confusing for parents, patients and health care practitioners to navigate. As such, this is an outline of a model of care that examines an integrated multidisciplinary approach to the life span management of AIS.
This article will narrow scoliosis discussion to the most predominant form which is Adolescent Idiopathic Scoliosis (AIS). AIS is characterized by curve development as a preteen that often progresses during the adolescent growth spurt which is approximately between 10-12 for girls and 14-16 for boys.
Timing of scoliosis treatment
Timing is critical for AIS management. If caught early as a tween, before the adolescent growth spurt, when curves are small and flexible, scoliosis treatment options are more numerous and have the greatest potential for halting or even reducing curve progression. As teenagers near maturity, when the spine stops growing, scoliosis treatment options quickly narrow.
To treat scoliosis you have to know scoliosis. You have to have an idea of why it starts and how it progresses. Once you know your opponent, you can in a sense, reverse engineer countermeasures and develop conservative and surgical treatment options if necessary. Then, you can match the appropriate treatment with specific patient maturity levels and scoliosis curve(s) severity to form a reasonably effective treatment plan.
But, scoliosis management and treatment doesn’t stop after bracing or after surgery. It continues for a lifetime. Scoliosis is an ongoing challenge between posture, sagittal/coronal curves and gravity.
The cause of scoliosis
Although the cause of adolescent idiopathic scoliosis is, by definition, unknown, it is generally accepted that the cause of AIS is genetic in origin.
I recently interviewed Dr. Rene Castelein MD, PhD from The Netherlands who focuses primarily on spinal deformity, both clinically and scientifically, especially in the field of etio-pathogenesis (or the cause) of idiopathic scoliosis. He has over 150 scientific publications to his credit and he gave me a much more thorough understanding of what triggers scoliosis and how it gets worse.
Scoliosis starts in the vertebral discs. It’s the combination of abnormal vertebral disc biomechanics and changes to the vertebral disc structure that drives scoliosis. Since change is “initially” in the discs, scoliosis is really a soft tissue disease and not a bone disease.
He hypothesized that as humans evolved from a quadruped to biped, the pelvis moved forward which shifted the body’s centre of mass posteriorly. This, in turn, makes the vertebral discs and adjacent vertebrae rotationally unstable.
This inherent rotational instability of the vertical human spine makes it more susceptible to the initiation and progression of scoliosis. When you simultaneously add other variables like changes to disc structure, poor collagen quality (hypermobility), flattening of the sagittal spinal curves in addition to a dysfunction of normal growth synchronicity between primarily the spinal discs and the rest of the body (arms/legs/head) you get scoliosis progression.
Sagittal alignment issues are coupled to disc rotation. As the spine rotates, the thoracic spine flattens becoming hypokyphotic. All scoliosis curves that are not due to structural vertebral issues, such as hemi-vertebrae or Schuerman’s Kyphosis, have some levels affected by hypokyphosis. This increases the height along the front of the spine (anterior column) relative to the back of the spine. To reduce the height of the anterior column, the spine goes into hypokyphosis, often lordosis, and the coronal curve buckles sideways producing a scoliosis curve.
In short, walking on 2 feet instead of 4 makes it easier for the discs to rotate out of place. At some point, synchronized chaos ensues. Collagen quality, flattening sagittal curves, teenagers’ arms and legs are growing at different rates to the spine which drives disc rotation and flat back eventually leading to scoliosis progression.
Reverse engineering scoliosis
Since scoliosis starts and then progresses with rotation of the vertebral discs and flattening of the spine, it makes sense that treatment options focus on trying to both derotate the spine and restore the normal kyphosis/lordosis alignment. This, of course, is difficult to address because there are many variables involved including age, the severity of curve(s), type of scoliosis, sagittal alignment and spine flexibility to name a few.
A recurring theme in this article will be: “early scoliosis monitoring and treatment increases the odds of success at all treatment stages whether it involves conservative treatment, bracing or surgical intervention.” Later treatment options narrow with age and severity of the scoliotic curve.
Scoliosis bracing
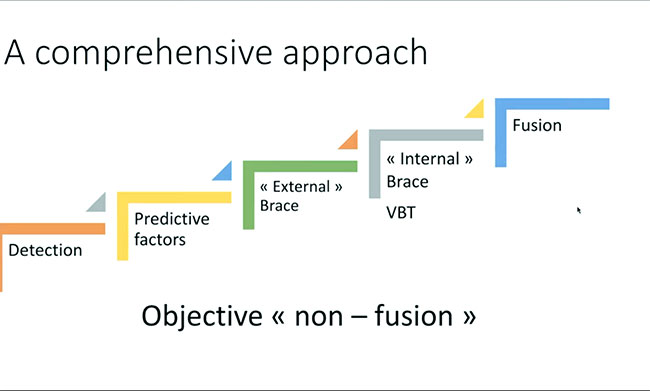
Dr. Aurélien Courvoisier, pediatric spine surgeon from Grenoble, France, sees conservative and surgical treatment of scoliosis as two opposite ends of a continuous spectrum. Appropriate bracing at the initial stages followed by non-fusion surgery if required with fusion surgery as the very last resort.
Dr. Courvoisier has excellent results (80% halting/reducing curve progression) with bracing kids with curves as low as 15 degrees (scoliosis diagnosis starts with a 10-degree curve with many surgeons waiting till 25-30 degrees to initiate bracing), especially if the child’s family has a history of severe scoliosis and if they are about to enter their growth spurt. These curves have a very high probability of rapid progression. Curves this small are often very flexible and malleable which lends itself to better bracing success.
Modern asymmetric derotation braces seem to be more effective than old-style symmetrical braces but the skill and experience of the orthotist is still paramount. While scoliosis bracing is improving in terms of attempting to derotate the spine, they still struggle to address the sagittal alignment of hyopkyphotic/lordotic thoracic scoliosis curves. Since disc/vertebrae rotation and spine hypokyphosis/lordosis are coupled motions, bracing and even surgery is a compromise because they are inversely related. Attempting to derotate discs/vertebrae with a brace can increase thoracic hypokyphosis/lordosis which can lead to curve progression, especially for stiff curves. The opposite is also true where trying to improve kyphosis can increase rotation leading to curve progression. Indeed, trying to brace stiff hypokyphotic/lordotic thoracic curves is often contraindicated.
As Dr. Manuel Rigo MD, inventor of the revolutionary Rigo Cheneau scoliosis derotation brace said, “Scoliosis, with potential for progression, is a constant and unpleasant lesson in humility.”
Patient compliance is the most important variable in bracing. The longer you wear the brace, the better the outcomes. Unfortunately, asking tweens and teenagers, mainly girls, to wear braces 18+ hours/day doesn’t bode well for compliance. I’m partial to Dr. Aurélien Courvoisier’s staged bracing protocol which favours high compliance as opposed to general North American bracing practices of jumping to maximum hours right away. Granted, this might also be due to the lack of school screening programs where curves are being diagnosed too late at already large curve angles.
In his practice, kids start early with nighttime bracing with 15-degree curves. If curves progress, bracing time increases to out of school bracing, limiting bracing to the home environment. Only for curves that are aggressive or that continue to progress will bracing increase to 18+ hours/day.
Chiropractic, naturopathic, physiotherapy scoliosis treatment
I’ve briefly discussed bracing but what about the role of chiropractic, naturopathy and physiotherapy and other healthcare practitioners? The same spectrum of treatment applies. There can be greater treatment impact with smaller more flexible curves. Especially so if there is a known family history of scoliosis.
Scoliosis research is continuously identifying genetic precipitators for scoliosis including melatonin deficiency to poor collagen and bone quality and opens opportunities for naturopathic intervention. Likewise, chiropractic scoliosis treatment protocols and physiotherapy-specific scoliosis exercises (Schroth, SEAS) can impact scoliosis, especially when the curve is mild, moderate and flexible.
When a curve is small and flexible, there are numerous treatment options. But these options fall by the wayside and quickly disappear as the curve progresses and often stiffens.
But, as I’ve learned the hard way, knowledge on the mechanics of scoliosis and experience plays a critical role in how a scoliosis patient is managed conservatively. Especially so when a curve keeps progressing into surgical range (50+ degrees) despite best efforts. Some scoliosis curves are going to progress no matter what we do. It’s our responsibility to identify when this is happening and then refer out for a surgical consultation.
Indeed, after interviewing 30 of the world’s top spine surgeons and talking to many more, it seems the ideal situation is to create a team of multidisciplinary health care practitioners including experienced scoliosis chiropractors, physiotherapists, naturopaths, orthotists and spine surgeons to manage and treat scoliosis patients through their journeys. If conservative treatment and bracing fail, then a surgeon is already involved and a seamless transition can be made if surgery is necessary.
But timing is everything when treating AIS. Even at the point of surgical intervention, there are options whether it be fusion or non-fusion.
Surgical scoliosis options: fusion and non-fusion
Spine surgeons are not created equal. Just like chiropractors, naturopaths and physiotherapists, we all vary in skill sets and levels of expertise and experience. The same is true for spine surgeons. One hundred percent of spine surgeons can offer fusion surgery to correct scoliosis. On the other hand, only a small percentage of spine surgeons, around 5-10%, are currently capable of offering non-fusion scoliosis surgery. In all of Canada, approximately 10 orthopedic spine surgeons offer both non-fusion and fusion scoliosis surgery.
Fusion surgery for scoliosis involves inserting screws into vertebral pedicles posteriorly and attaching corresponding metal rods. The spine is de-rotated and a normal sagittal alignment is attempted. Bone chips are added to the exposed posterior column and the spine fuses as one mass for the length of instrumentation.
Although this is currently the gold standard for scoliosis surgery, adjacent segment degeneration (ASD) is common above and below the fused levels leading to faster disc and facet joint degeneration. This is much more common for lumbar fusions especially as levels are fused toward the sacrum as lumbar spine flexibility is lost. This may necessitate additional fusions to stabilize levels that have degenerated. Thoracic only fusions have a better long-term track record with less ASD due to the inherent stiffness of this part of the spine.
A relatively new surgical procedure, which does not involve fusion, called Vertebral Body Tethering (VBT), involves inserting screws anterolateral into the vertebrae along the convex side of the scoliosis curve. A polyethylene cord or tether is attached to the screw heads and tensioned thereby straightening the curve typically by 50%. Additional straightening of the curve is seen with continued passive growth of the spine to maturity. At maturity, bone growth modulation of the vertebrae will stabilize the tethered levels. The goal of this non-fusion technique is to avoid fusion. Revision rates are 10-15% due to tether ruptures and or overcorrection of the curve if the adolescent grows too quickly.
When a scoliosis non-fusion/fusion surgeon is part of the team early on, then that surgeon may have non-fusion surgical options available like VBT which are appropriate, in general, for adolescents during their growth spurts. Anterior Scoliosis Correction (ASC) is generally extending VBT to mature spines that have reached maturity.
Understanding Scoliosis
Once you understand scoliosis, you can reverse engineer countermeasures and develop conservative and surgical treatment options. Then, you can match appropriate treatment options with specific patient maturity levels and scoliosis curve(s) severity to form a reasonably effective treatment plan.
As Dr. Courvoisier mentioned, he proposes a “comprehensive” approach to treating scoliosis with conservative treatment on one end and surgical intervention at the other end of the spectrum. Even this approach is not widely implemented for scoliosis care although it should be.
But, taking this a step farther, scoliosis management doesn’t just stop after the spine stops growing and matures. Management of scoliosis doesn’t stop post bracing or post-surgery whether it be non-fusion or fusion.
Side effects of scoliosis
Indeed, there is a multitude of side effects that ripple from the spinal curves impacted by scoliosis. The lumbar and cervical spines are typically impacted with the loss of cervical spine lordosis that often reverses into kyphosis. Early cervical and lumbar disc degeneration can often be seen in adolescents.
Once again, regardless of conservative treatment including bracing or surgical intervention, these spinal junction areas need care. This is an obvious opportunity for chiropractors, naturopaths and physiotherapists to work on posture, spine flexibility, strength and nutrition on an ongoing basis.
Conclusion
Ideally, I’d like to see a multidisciplinary team of healthcare practitioners bring their specific skills and experience at the right time on the treatment spectrum. Surgeons are integrated at detection but monitoring, especially through the adolescent growth spurt to intervene if conservative treatment fails with both non-fusion and fusion surgical options.
Right now, scoliosis treatment is mostly narrow in breadth, disconnected among disciplines and confusing for parents, patients and healthcare practitioners to navigate. There is much work to do, but a comprehensive multidisciplinary approach to managing and treating scoliosis is more than worth the effort.
Print this page