
In part one (“Life and Longevity: Serious health issues, and an opportunity to lead” June, 2020) we looked at the aging population data, and how the unique characteristics of aging can contribute to major health issues and begin the progression for the development of:
Impairment -> Functional Limitations -> Disability.
After undertaking the standard consultation/physical, one understands the patient’s condition and has some information on the physical/cognitive aspects of their problem. But, this may not be adequate when dealing with the aging person. Take muscle testing in a supine/prone position, as an example. However, we also operate in a dynamic mode, we sit, stand, walk, reach, open doors, carry things, get in cars and drive them.
As you can see, there are gaps in the standard consultation/physical model, especially when dealing with the aging population. If one were to add to the previous example, simple functional assessment scales, which are easy to use, and proven valid and reliable, then we obtain a more functional picture of the aging person. These simple functional assessments will also provide us with objective base line data, so we can be specific regarding the main issue(s) for the patient, and design a program to improve the main issue(s). We can also use the baseline data to monitor progress and to decide if we need to change programs. This is better for the patient, and from a professional perspective, more rewarding for the doctor.
For instance, let’s look at balance. It is a common issue as we age and some of the contributing factors could be the following: Sedentary lifestyle, foot problems, lower limb muscle strength, osteoarthritis of the knee or hip, fear of falling, not walking properly, feeling one foot more on the floor than the other, postural torsion, not feeling energized and worrying. This can in turn lead to: Altered gait, shuffling gait, stopping exercising, decreased agility, decreased socializing, depression, anxiety, stopping cooking, no regular meals and sarcopenia.
By utilizing one or all of the following four assessments tools outlined below, let us see if they can give us useful information regarding impairment and or functional limitations regarding the patient. Safety, when functionally assessing the aging patient is very important.
An outline of the assessment tool will be presented and a summary of its pertinent findings highlighted.
Berg Balance Scale (1)
Measures Balance in older adults and consists of 14 items:
- Sitting to standing
- Standing unsupported
- Sitting unsupported
- Standing to sitting
- Transfers
- Standing with eyes closed
- Standing with feet together
- Reaching forward with outstretched arms
- Retrieving object from floor
- Turning to look behind
- Turning 360 degrees
- Placing alternate foot on stool
- Standing with one foot in front
- Standing on one foot
Summary: It takes about 10 minutes and provides functional objective data on lower limb strength, moving between locations, ability to stand with eyes closed/feet together, bending over to pick things from the floor, turning around and looking behind while walking, ability to raise one foot and body balance on one foot. This is a lot of information from 10 minutes of testing.
Senior Fitness Test Battery (2)
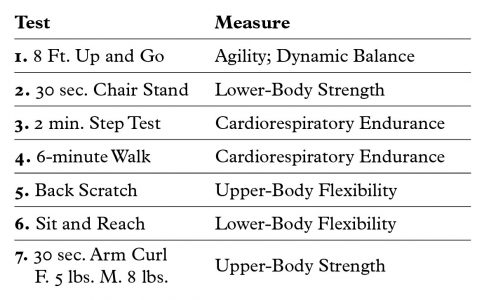
This test battery consists of 7 tests that measure muscular strength, flexibility, cardio- respiratory endurance and dynamic balance/agility. Each test has been proven to be valid and reliable for use with the older population.
Summary: It takes about 12 minutes and provides functional objective data on agility and movement, upper/lower body strength, cardiovascular endurance and flexibility. This test is more comprehensive and gives the Doctor insight into mental/cognitive toughness.
Rapid Geriatric Assessment (3)
The Rapid Geriatric Assessment (RGA) measures frailty, sarcopenia, anorexia, cognition, and advanced directives. The RGA is a screen for primary care physicians to be able to detect geriatric syndromes.
Summary: This takes about 5 minutes and is used to identify early intervention when geriatric syndromes are present.

Dealing with osteoarthritis, how do we begin to strengthen the weak muscles caused by the OA? Photo: staras/Adobe stock
Modified Clinical Test of Sensory Interaction in Balance (4)
This test is designed to assess how well an older adult is using sensory inputs when one or more sensory systems are compromised. mCTSIB is a simplified test which assesses the patient’s functional balance control during four sensory conditions. Although the mCTSIB data set can document the presence of sensory dysfunction, it cannot provide impairment information specific to an individual sensory system. mCTSIB quickly assess the role of the visual, somatosensory and vestibular systems.
Here are the steps:
- Eyes open firm surface (3/3 i.e. vision, somatosensory, and vestibular)
- Eyes closed firm surface (2/3 i.e somatosensory, and vestibular)
- Eyes open unstable surface (foam) (2/3 i.e., vision, and vestibular)
- Eyes closed unstable surface (foam) (1/3 i.e., vestibular)
Summary: It takes about 5 minutes and provides information regarding which system the patient depends on and which may be weak. Be very careful with this assessment. One has to “cage” the patient at all times. Patients can fall over, or just collapse when doing item #4.
Obtaining information from the Physical/Consultation and Functional Assessment tools, will provide the doctor with a comprehensive picture regarding the contributing factors, and may identify the system most in need of specific interventions. One will also have baseline data to monitor progress, or the efficacy of the therapeutic interventions. Examples are numerous. Balance problems have been corrected by treating patients’ feet – part of the somatosensory system, or by addressing the visual system – teaching them to look ahead and utilize more of their peripheral vision.
We need to take an integrative approach, focusing on the system’s capabilities. We have to be cognizant that all systems interact with each other and can affect each other. As an example, osteoarthritis – OA, affects over 20% of people over 60 years old. OA of say the knee, causes weakening of muscles at the specific joint, altered biomechanics of the joint, affects mobility, postural mechanics and may cause the person to take pain killers. As the OA progresses, physical activity is curtailed, sleep maybe compromised, social activities decline, weight may increase and cognitive functions begin to decline.
To begin to treat this patient, we need to gather all the information as per above. We have to focus on the OA of the knee, taking into consideration all of the other systems, cognitive, posture, muscle strength, gait, balance, diet and how it has affected the patient socially. But more specifically, dealing with the OA, how do we begin to strengthen the weak muscles caused by the OA? Also of importance, one should note if there are weaknesses of the lower limb muscles that are salient to the aging process. Do we assess and begin to correct the mechanics of the lumbo pelvic area; the hips; the feet? Do we use nutritional supplementation initially to assist with the inflammation? What lifestyle changes do we recommend to start the process? What type of exercises do we begin with: stretching/flexibility; thera band; body weight, balance training; resisted exercises with weights; endurance exercises or power exercises?
The next article will address a general approach regarding how to treat/train the lower body muscular system. We will address which muscle fiber is most compromised, which key muscles get weak due to the aging process. Does one treat/train for strength or power?
References
- Lusardi M. Functional Performance in Community Living Older Adults. J Geriatric Phy Therapy. 2004, 26(3), 14-22.
- Rikli R, Jones J. Development and Validation of Criterion-Referenced Clinically Relevant Fitness Standards for Maintaining Physical Independence in Later Years. Gerontologist, Apr 2013, 53 (2), 255-67.
- Morley J. Rapid Geriatric Assessment: Secondary Prevention to Stop Age-Associated Disability. Aug 2017 Clin Geriatr Med, 33 (3), 431-440.
- Park M, Kim K, Evaluation of Uncompensated Unilateral Vestibulopathy Using the Modified Clinical Test for Sensory Interaction and Balance. Otol Neurotol, Feb 2013, 34 (2), 292-6.
Dr. Don Fitz- Ritson is a chiropractor and a rehab specialist. He was an Assistant Professor at CMCC. He published 17 papers and 3 chapters on chiropractic.He co-invented a laser and it received 7 Health Canada Approvals. He is focused on helping the aging population live better lives.
Print this page
