
Improve spinal function to promote the patient’s return to activities.
Do you feel stressed or frustrated when certain chronic pain patients come into your clinic? If so, then you might consider a new paradigm for treating chronic pain. Guideline literature has demonstrated the effectiveness of chiropractic treatment of acute low back and neck pain. What about chronic pain? There has been little evidence to substantiate that chiropractic adjustments alone are effective in treating chronic pain. However, guidelines suggest that, with a specialized approach to patient management, chiropractors have the potential to make a strong contribution in the field of chronic pain.
A DEFINITION
Chronic pain is usually defined as pain that persists one month beyond the resolution of an acute injury, pain that continues or recurs for longer than three months, or tissue injury pain that is expected to continue or progress. Chronic pain tends to not be responsive to the interventions that usually resolve acute pain. It is often associated with comorbid medical or psychological conditions and with functional impairments.
Demographics show that, at any given time, approximately 5% of the population experiences acute pain. Due mostly to degenerative changes, the rate of chronic pain is shown to increase with age, from 10% by age 40 to 20% by age 60, and to 30% from the ages of 70 to 80.
 PARADIGM FOR THE MANAGEMENT OF PAIN
PARADIGM FOR THE MANAGEMENT OF PAIN
Acute pain is simpler to treat because success is measured by resolution of pain. When pain becomes chronic, things become more complicated. If your entire treatment revolves around pain management, then you and the patient will become frustrated with the constant ups and downs and good and bad days of the chronic pain disorder.
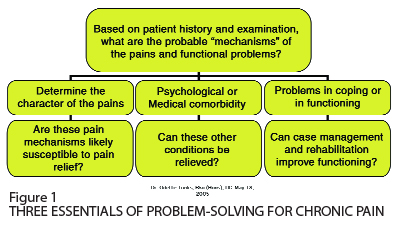
Whether it is the elite athlete presenting with chronic rotator cuff pain, the elderly person with arthritis, or the injured worker with chronic low back pain, the emphasis should be on improving spinal function to support return to activities. A simple and effective management strategy is diagrammed in Figure 1.
MECHANISM OF PAIN AND PAIN RELIEF
As primary health-care practitioners, it is important that we perform a thorough history and examination to determine the mechanism of the pain. Appropriateness of treatment depends upon the pain mechanism. If the pain problem is purely mechanical in nature, then mechanical treatments are in order – and chiropractors are experts in this field.
Chiropractors also play a vital role in identifying certain specialized chronic pain conditions that require medical intervention. For example, nerve pain may on closer examination reveal the classic signs of neuralgia (hyperpathia, hyperalgesia, and allodynia) for which a physician might prescribe anticonvulsant medication. Signs and symptoms may suggest compression fractures due to osteoporosis. Identification of red flags for cancer or other pathology might, with earlier diagnosis and referral, represent the difference between life and death for a patient. A sudden onset of “new” or “different” back pain in an elderly patient raises the possibility of pathology such as fracture or cancer. Patients may present with a combination of symptoms that suggest systemic disease, such as systemic lupus erythemetosis, rheumatoid arthritis, ankylosing spondylitis, multiple sclerosis, etc.
As a chiropractor, you are an expert in the diagnosis and treatment of neuromusculoskeletal disorders, and your patients are grateful, not just for your treatment, but also for your appropriate referrals when necessary.
PSYCHOLOGICAL, PSYCHOSOCIAL AND MEDICAL COMORBIDITY
While treatment of pain is important to the chronic pain patient, good literature demonstrates little success in treating their chronic pain with passive therapies alone. Part of the reason for this is that chronic pain patients often also suffer from comorbid psychological, psychosocial or medical problems that need to be addressed.
Psychosocial problems may include low self-esteem, family discord, workplace or financial stress, etc. Patients may also present with medical comorbidities such as obesity, diabetes, deconditioning, sleeping disorders, and alcoholism/addictions.
Though it is outside our scope of practice to diagnose psychiatric and medical disorders, it is our responsibility as primary health-care providers to look at the patient as a whole. Psychological factors can be identified by asking standard questions during the history taking (Figure 2). Referral to the family physician for further investigation may be warranted in the case of patients who exhibit some of the signs and symptoms. Depression, dysthymia, and anxiety are among the more common psychological comorbidities, which will interfere with the chronic patient’s ability to cope with the pain and their functional loss.
As chiropractors, we may often help patients with issues such as weight loss, nutrition, sleeping disorders, deconditioning, low self-esteem, or other simple psychosocial and medical issues. Certain comorbidities can be addressed by the chiropractor, and some need to be treated elsewhere.
When teaching, I am frequently asked, “How do you approach the subject of depression or anxiety with a patient so they don’t take it the wrong way?” The answer is that you need to be respectful, clear and informative. While presenting my report of findings, I might say, “It is very common with any type of chronic pain for people to experience depression. Some of your answers today indicate that you are feeling downhearted and sad (give examples). It is important to talk to your family doctor about these feelings, and if you like I will write a letter to let him/her know what we have discussed.”
Patients will appreciate that you have taken the time to ask them about how they are feeling, and that you understand the psychological impact of chronic pain.
CHIROPRACTIC TREATMENT OF FUNCTIONAL PROBLEMS
Often patients seek treatment because chronic pain is interfering with their sports activities, work, caregiving, household chores, or social life. The goal of chiropractic treatment is to improve function, despite pain. Certainly, adjustments and soft tissue therapy will help to manage pain and improve mobility, but the emphasis should be on improving spinal function to support a return to activities. Educate patients on exercise. Let them know that you will provide the manual therapy that will allow them to perform their exercises more comfortably, improve their range of motion, and thus get them back to work or daily activities more quickly, depending on each patient’s unique goals.
Help the patient with their goal-setting, and suggest they record their progress by keeping a diary. Goals need to be specific and reasonable, such as, “I want to be able to walk five minutes per day, increasing by one minute per week,” or “I want to be able to do the laundry once per week.” Conversely, “I want to feel better and do everything I did before” is neither specific nor reasonable. Recommend graduated exercise programs and a measured return to activities using appropriate pacing strategies that include short breaks. Evidence suggests that the individual ought to return to activities “as tolerated,” not pushing into the pain. Going back to work should not be delayed since a prolonged absence lowers the likelihood of successful work re-entry. A modified job description and availability of light duties will promote success.
Chronic pain management is critically important in the working population. A majority of work-injured employees (75%) return to work in two to three weeks. All but 7-10% have not gone back within six months, but this small group of accounts for 75-80% of the cost to the system through lost work hours, indemnities, and health-care usage. Psychosocial factors are significant in these workers. Studies on whiplash and low back pain with sciatica have found similar recovery patterns.
Recently, the Workplace Safety and Insurance Board (WSIB) of Ontario approved maintenance care, due to evidence that chiropractic and other passive forms of therapy are effective for chronic pain when they promote activation and function. Likewise, insurance companies will endorse chiropractic care for a chronic pain patient if treatments are required to support the individual’s activity and function.
Since your patient with chronic pain will have good and bad days, the barometer of treatment success should not correlate with pain levels, or you will both be riding an eternal rollercoaster.
The paradigm described in this article suggests a better way to measure improvement and success: find the mechanism of the pain so that pain can be appropriately treated; identify possible co morbidities for treatment or referral onwards; and focus on the promotion of activity and function.
Instead of asking about the patient’s pain level that day, inquire about how they are getting along with their sports, laundry, dusting, walking, and sleeping. Stay positive and help patients be aware of what they can do, not what they can’t.•
Print this page