
Facts on Facet
By Richard Brownlee
Features Clinical TechniquesDiagnosis, treatment of facet joint syndrome
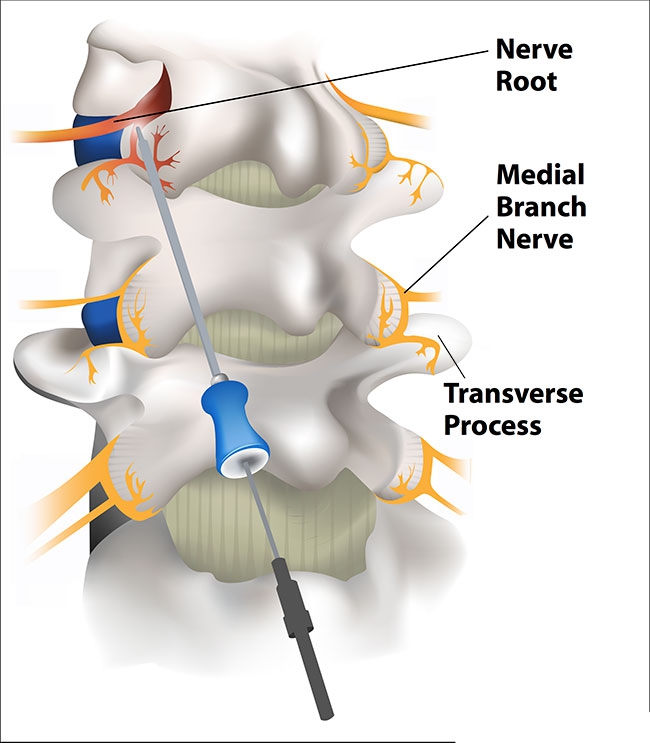 Artist’s drawing of the posterior aspect of the lumbar spine showing the medial branch nerves (yellow) innervating the facet joints. The cannula and electrode are positioned on the medial branch nerve of the painful facet joint (red) where a radiofrequency lesion is created to denervate the joint and relieve the pain. Illustration: Haley Fulton
Artist’s drawing of the posterior aspect of the lumbar spine showing the medial branch nerves (yellow) innervating the facet joints. The cannula and electrode are positioned on the medial branch nerve of the painful facet joint (red) where a radiofrequency lesion is created to denervate the joint and relieve the pain. Illustration: Haley FultonBiomechanics is the study of motion and related forces in biological systems including the spine. The spine is composed of an anterior column of vertebrae and discs and a posterior arch of bone that surround and protect the spinal cord and nerve roots. The discs are cushions that act as shock absorbers during axial loads placed on the spine.
The zygapophyseal or “facet” joints are paired structures that lie posterolaterally between each spinal segment. The muscles, ligaments and tendons attach to the bony elements of the spine and help provide stability.
The nervous system orchestrates movement in different directions through the muscles, which act upon the spine. It is the facet joints that control the extent of spinal motion. The facet joints are susceptible to the same types of injury, inflammatory and degenerative processes that affect other synovial joints throughout the body, which can result in pain.
It is often difficult or impossible to identify the exact source of spine pain because different structures may be involved in pain generation. Facet joint pain can usually be relieved by chiropractors through their training in palpation and adjustments of the spine. This article describes the basic anatomy of the lumbar facet joints, their nervous innervation, and minimally invasive procedures that can be used to identify a painful facet joint and provide pain relief.
Anatomy
Facet joints are synovial joint that are formed between the lateral facing inferior articular process and the medial facing superior articular process of adjacent vertebrae. They form part of the posterior arch of bone and are extensions of the lamina of each spinal segment. There are 24 vertebrae (C1 to S1) and 23 pairs of zygapophysial joints from cervical C1-2 to lumbar L5S1 levels, which are involved in spinal motion. The orientation of the joints changes from being almost horizontal in the cervical spine to a progressively more oblique orientation in the lumbar spine.
The size of the joints also increases from the cervical to the lumbar region. The orientation of the joints controls the amount of flexion, extension and rotation that occurs at different segments of the spine. They also prevent forward sliding of adjacent vertebrae and lateral displacement of the posterior elements.
Each facet joint consists of a superior and inferior articular process that is lined by a thin, smooth layer of cartilage. A synovial membrane attaches along the peripheral margin of the cartilage and maintains a thin layer of synovial fluid within the joint space.
Facet joints are endowed with intra-articular meniscoids that are composed of adipose tissue and blood vessels. They are located at the superior and inferior poles of the joint. The posterior surface of the joint is enclosed in a fibrous capsule of collagen fibers. The anterior surface is formed by the ligamentum flavum, which is a lateral extension of the interlaminar ligament.
Innervation of facet joints
The sensory innervation to the facet joint is consistent. The spinal nerves at each level exit the intervertebral foramen and divide into anterior and posterior primary rami. The posterior ramus, in turn, divides into a lateral branch that innervates the paraspinal muscles and a medial branch that provides sensation to the facet joints.
The medial branch nerve runs across the top of the transverse process at its junction with the superior articular process. Each facet joint receives sensory innervation from the medial branch nerve at the same vertebral level and from a descending branch from the level above. For example, the L4-5 facet joint is innervated by the L3 medial branch, which crosses the L4 transverse process and the L4 medial branch nerve, which crosses the L5 transverse process. The L5S1 facet joint is innervated by the L4 medial branch, which crosses the L5 transverse process and the L5 dorsal ramus, which crosses the Sacral Ala.
To remove sensation from a painful facet joint, two medial branch nerves have to be anesthetized (blocked). The medial branch nerves also innervate the multifidus muscle, the interspinous muscle and interspinous ligament at the same segmental level as the named medial branch nerve.
Changes with injury and aging
Repeated stresses applied to the joints lead to progressive changes that may be classified as osteoarthrosis. This is not a disease but an expression of the morphologic consequence of stresses applied to the joints over time.
Imaging studies with x-ray, CT and MRI often reveal changes, which include erosion and focal thinning of the cartilage, osteophyte formation at attachment sites of the capsular ligaments or ligamentum flavum, synovial cyst formation and enlargement of the joints. These changes occur with equal frequency in patients who have back or neck pain and in those who do not have pain. Patients who have normal appearing facet joints can also experience pain. Therefore the source of a person’s pain cannot be determined solely by the morphologic appearance of the joints on imaging studies.
Facet joint syndrome
The lumbar facet joints are a recognized source of low back pain and referred leg pain. The term, facet syndrome was coined by Gormley in 1933. The prevalence of facet joint pain is reportedly between 15 and 40 per cent of people who suffer from chronic low back pain. Facet joints are a common source of neck pain following whiplash injury. While there is no pathogneumonic sign or symptom that distinguishes facet joint pain, it is generally accepted that facet joint pain is aggravated by extension and standing, as opposed to discogenic pain, which occurs with forward flexion or sitting. In addition to chronic back or neck pain, facet joint pain often occurs in episodic, severe exacerbations of pain that can last for days.
People with facet joint pain often report collapsing or becoming completely immobilized by their pain.
Diagnostic blocks
Determining if pain is arising from the facet joints and which joint is the source of the pain can be done through diagnostic medial branch blocks. This involves the injection of local anesthetic under x-ray guidance, onto the nerves that transmit pain from the joints to the brain. Each medial branch nerve is located at the junction of the transverse process and superior articular process, and each facet joint is innervated by two medial branch nerves. Therefore, both nerves must be anesthetized to determine if the pain is arising from a particular facet joint.
For example, to anesthetize the L4-5 facet joint, a small volume of local anesthetic is injected onto the transverse processes at the L4 and L5 levels. To be positive, the injection of local anesthetic should provide complete relief of pain for the duration of action of the local anesthetic agent used. Intra-articular injections of local anesthetic and steroid can provide pain relief of variable duration but have not been shown to be reliable as a diagnostic procedure, as they do not provide anesthesia to the two medial branch nerves.
Treatment
Medial branch neurotomy, which is also referred to as facet joint rhizotomy can provide more long-term pain relief than steroid injections. Facet joint rhizotomy is a minimally invasive surgical procedure performed under fluoroscopic x-ray guidance. A cannula is inserted through the skin and advanced onto the transverse process at its junction with the superior articular process of the facet joint. The cannula consists of an 18 or 20 gauge needle that has an insulated covering over all except the last one-centimetre portion of the needle. An electrode is inserted into the cannula.
An OWL radiofrequency generator is used to pass an electric current through the electrode. Sensory and motor stimulation are performed to reproduce their back pain and to ensure there is no muscle contraction in the leg. Radiofrequency thermocoagulation of the medial branch nerves is achieved by heating the tissue surrounding the exposed, non-insulated portion of the cannula to a temperature of 80 C for 120 seconds. This denatures the medial branch nerve and prevents it from transmitting the pain signal to the dorsal root ganglion and on to the brain.
Radiofrequency ablation of the two medial branch nerves to a facet joint usually results in pain relief for approximately one year. The procedure can be repeated if the pain recurs. Complications are uncommon but patients can experience an exacerbation of their pain following the procedure that can last for several days before they achieve the expected pain relief.
Facet blocks and rhizotomies can be performed on the cervical, thoracic and lumbar spine.
Dr. Richard Brownlee is a neurosurgeon running a combined cranial and spinal neurosurgery practice in Kamloops, B.C. since 1996. He was president of the medical staff and chief of surgery at Royal Inland Hospital, and currently president of the Welcome Back MRI and Pain Management Centre in Kamloops, a multidisciplinary medical clinic with the only upright MRI machine in Canada and a fluoroscopy suite for diagnostic and therapeutic pain procedures.
Print this page